The Humble Beginnings of Clinical Research
Clinical research has its origins in the ancient world, dating back to 2737 BCE. In 2737 BCE, the legendary Chinese emperor Shen Nung is considered the father of Chinese medicine. He purportedly experimented with and classified hundreds of medicinal herbs, conducting a number of studies with them. It was this first attempt at systematic experimentation that laid the groundwork for the growth of the clinical research that followed.
Centuries later, in the Old Testament, the book of Daniel describes what could be considered the first recorded clinical trial. Under the rule of King Nebuchadnezzar II, children of royal blood and certain children from conquered Israel were recruited to be trained as the king’s advisors.

Daniel, however, requested that he and three other Hebrew children be allowed to have only legumes and water, rather than the king’s meat and wine. After a 10-day trial period, Daniel’s group was noticeably healthier than the group on the king’s diet, and they were permitted to continue their regimen for the entire training period.

As the centuries passed, the field of clinical research continued to evolve, with notable milestones and advancements. In 1537, the French surgeon Ambroise Paré accidentally conducted a clinical study when he ran out of his standard treatment for gun wounds and used a different mixture, which he observed to be more effective.
In 1747, the Scottish physician James Lind conducted a systematic experiment on the treatment of scurvy, discovering that citrus fruits were the most effective remedy.

The Emergence of Modern Clinical Research
The 20th century saw a significant transformation in clinical research. In 1863, the US physician Austin Flint conducted the first study with a placebo, testing a substance with no therapeutic effect on prisoners with rheumatic fever and comparing their response to that of patients who had received an active treatment. This marked a crucial step in the development of clinical trial methodology.
The 1920s brought the introduction of randomization, a technique that involves randomly assigning participants to different treatment groups, including a placebo group. This helped to minimize bias and ensure the validity of the results. The 1940s saw the emergence of blind clinical trials, where neither the participants nor the researchers know which treatment is being administered. The first double-blind controlled trial, on the treatment of the common cold, was conducted during this period.
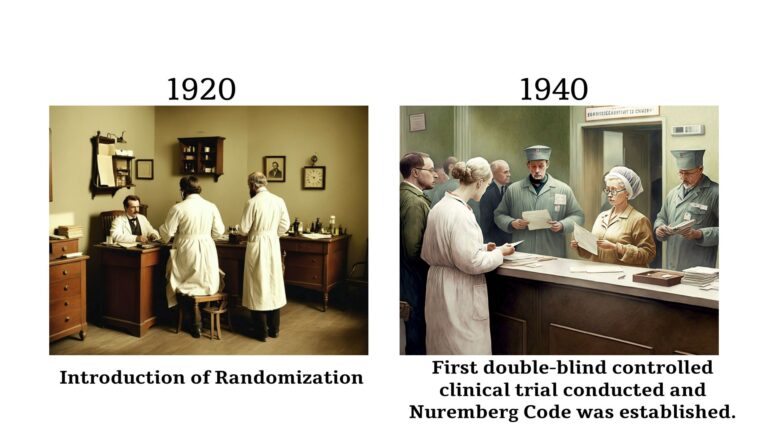
The 1940s also witnessed a significant milestone in the history of clinical research: the Nuremberg Code. Developed in the aftermath of World War II, the Nuremberg Code outlined 10 basic principles for the protection of human participants in clinical trials, including the requirement of voluntary consent and the avoidance of unnecessary harm. This landmark document laid the foundation for modern research ethics.
In the following decades, the field of clinical research continued to evolve, with the introduction of the Declaration of Helsinki in 1964, which further strengthened the ethical guidelines for the conduct of clinical trials. The 1980s saw the establishment of the International Conference on Harmonization (ICH), which aimed to harmonize drug development requirements across the European Union, Japan, and the United States. This paved the way for increased efficiency and improved availability of new drugs to patients.
Lessons Learned: The Importance of Ethics in Clinical Research
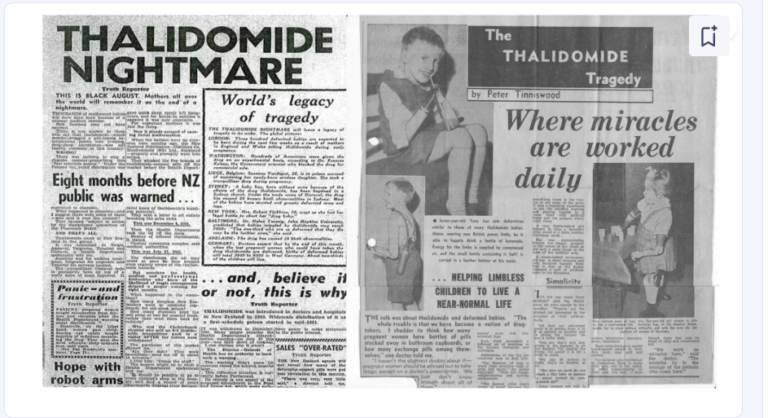
The remarkable progress in clinical research has not been without its challenges. Tragic events, such as the thalidomide disaster and the Tuskegee syphilis study, have served as painful reminders of the importance of ethical considerations in clinical research.
The thalidomide disaster, which occurred in the late 1950s and early 1960s, brought to light the weaknesses in the regulatory process for drug development and marketing. Thousands of babies were born with severe deformities due to the use of thalidomide during pregnancy, leading to stricter regulations and the requirement of rigorous clinical trials before drug approval.
The Tuskegee syphilis study, conducted by the United States Public Health Service between 1932 and 1972, was an egregious violation of ethical principles. Hundreds of African-American men with syphilis were deliberately denied treatment, even after the introduction of penicillin as a cure, in order to study the natural progression of the disease. This study, which caused immense suffering and loss of life, led to the establishment of the Belmont Report and the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research.
The Belmont Report, published in 1979, outlined three core ethical principles that should guide the design and review of clinical trials: respect for persons, beneficence, and justice. These principles, along with the Nuremberg Code and the Declaration of Helsinki, have become the foundation for modern research ethics, ensuring the protection of human participants and the integrity of clinical research.

The Evolving Landscape of Clinical Research
The field of clinical research has continued to evolve, adapting to new challenges and opportunities. The globalization of clinical research has brought both benefits and ethical considerations, as researchers must navigate diverse regulatory environments and cultural contexts. The rise of contract research organizations (CROs) has introduced new models for conducting clinical trials, with both advantages and potential drawbacks in terms of workforce qualifications and data ownership.
The relationship between academia and industry has also undergone significant changes. The Bayh-Dole Act of 1980 in the United States paved the way for increased collaboration between universities and the private sector, allowing for the commercialization of discoveries made through federally funded research. This has led to a surge in industry sponsorship of clinical trials, as companies seek to translate academic research into marketable products.
However, this partnership has also raised concerns about potential conflicts of interest and the influence of commercial interests on the design, conduct, and reporting of clinical trials. Researchers and institutions must navigate these complex dynamics, ensuring that the pursuit of scientific knowledge and the well-being of research participants remain the top priorities.
The Future of Clinical Research: Embracing Innovation and Ethical Stewardship
As we look to the future, the field of clinical research faces both challenges and exciting opportunities. The increasing complexity of drug and device development, the need for greater transparency and reproducibility, and the ongoing quest for personalized medicine all require innovative approaches and a steadfast commitment to ethical principles.
Technological advancements, such as the use of real-world data, artificial intelligence, and digital health tools, have the potential to streamline clinical trials, improve patient recruitment and retention, and enhance the collection and analysis of data. At the same time, these new technologies bring their own set of ethical considerations, requiring careful oversight and the development of robust guidelines.

The role of the researcher in this evolving landscape is more crucial than ever. Clinicians and scientists must not only possess technical expertise but also demonstrate strong leadership, authenticity, and a deep understanding of the ethical implications of their work. By fostering a culture of integrity, collaboration, and a relentless pursuit of knowledge, the clinical research community can continue to drive medical progress while upholding the highest standards of ethical conduct.
The journey of clinical research, from its ancient roots to the modern marvels of today, is a testament to the human spirit of inquiry and the unwavering commitment to improving the human condition. As we move forward, the lessons of the past and the ethical principles that have been hard-won must guide us, ensuring that the advancement of scientific knowledge is always balanced with the protection and well-being of those who participate in clinical trials. The future of clinical research holds the promise of transformative discoveries, but it is our responsibility as a global community to ensure that this progress is built on a foundation of ethical stewardship and a steadfast dedication to the betterment of humanity.

